The treatment of a child‘s cough or difficult breathing will depend on your assessment and classification of their illness. This section looks at the different treatments depending on the level of classification.
Treatment for severe pneumonia or very severe disease
A child classified as having severe pneumonia or very severe disease is seriously ill. The child needs urgent referral to a health centre or hospital for treatments such as oxygen or injectable antibiotics. Before child the leaves the health post, you should give the child first dose of Cotrimoxazole/Amoxicillin. The antibiotic helps prevent severe pneumonia from becoming worse.Then refer the child urgently to the hospital.
Treatment for pneumonia
If you have classified the child as having pneumonia you can treat the child him or her in your health post. The child needs treatment with antibiotics if there is no other classification for a referral.
Among the three types of Cotrimoxazole formulations, choose the one that is available in your health post (see table below).
Table 4.2. Cotrimoxazole antibiotic dosage for pneumonia and pre-referral treatment.
| COTRIMOXAZOLE (Trimethoprim + Sulphamethoxazole) Give two times daily for five days. |
|||
| AGE or WEIGHT |
ADULT TABLET 80 mg Trimethoprim + 400 mg Sulphamethoxazole |
PAEDIATRIC TABLET 20 mg Trimethoprim + 100 mg Sulphamethoxazole |
SYRUP 40 mg Trimethoprim + 200 mg Sulphamethoxazole per 5 ml. |
| 2 months up to 12 months (4 - 10 kg) |
1/2 | 2 | 5 ml |
| 12 months up to 5 years (10 - 19 kg). |
1 | 3 | 7.5 ml |
| Amoxicillin Give 3 times daily for 5 days |
||
| AGE or WEIGHT |
Tablet 250mg |
Syrup 125mg /5ml |
| 2 months up to 12 months (4 -10 kg) |
1/2 | 5ml |
| 12 months up to 5 years (10 - 19 kg). |
1 | 10ml |
Treatment for a chld with NO pneumonia: a cough or cold
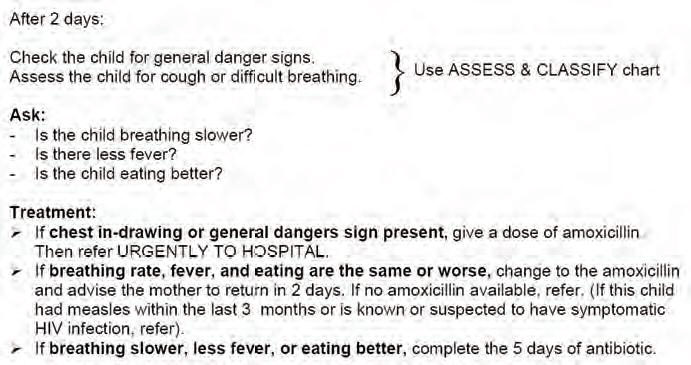
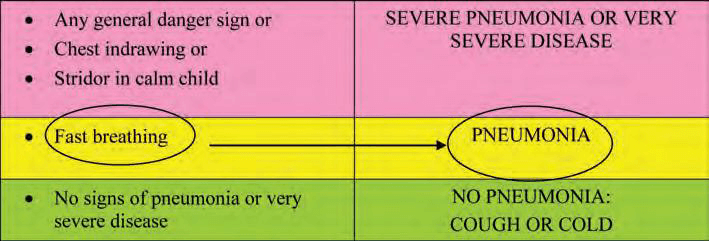
Follow-up care for pneumonia
If a child has been classified with pneumonia, it is important that the mother is told to return to the health post in two days‘ time for a follow-up visit. The health extension worker should assess the child for a cough or difficult breathing in the way outlined in the box below
The following case study will help you check your understanding what you have read so far in this study session.
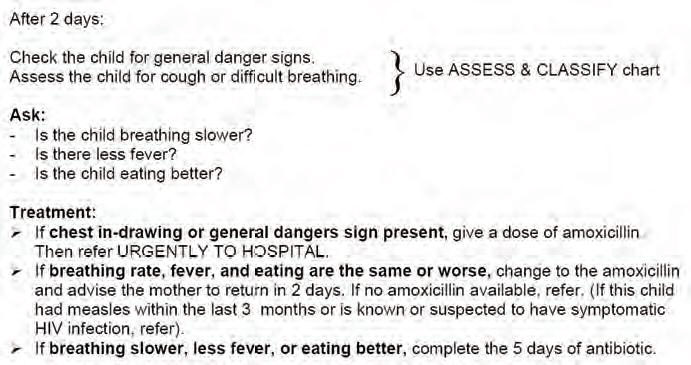
Aziz is 18 months old. He weighs 11.5 kg. His temperature is 37.5°C.His mother brought him to the health post because he had coughed. She says he was having trouble breathing. This is his initial visit for this illness. The health extension worker checked Aziz for general danger signs
The health extension worker (HEW) asked the mother, "How long has Aziz Had this cough?" His mother said that Aziz had been coughing for six or seven days. Aziz sat quietly on his mother‘s lap. The HEW counted the number of breaths the child took in a minute and counted 41 breaths. She thought, ‗Since Aziz is over 12 months of age, the cut-off for determining fast breathing is 40. He has fast breathing‘. The HEW did not see any chest in-drawing. She did not hear stridor. The chart below shows you how the HEW recorded Aziz's case information and signs of illness. To classify Aziz‘s illness, the HEW looked at the classification table for coughs or difficulties in breathing.
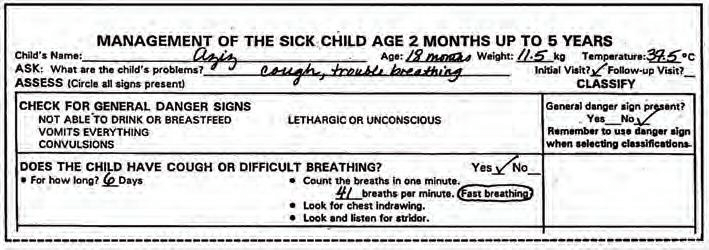
First, she checked to see if Aziz had any of the signs in the pink row. She considered, "Does Aziz have any general danger signs? No, he does not. Does Aziz have any of the other signs (chest in-drawing and stridor in a calm child)in this row? No, he does not. Therefore Aziz does not have any of the signs of severe pneumonia or very severe disease."
Next, the HEW looked at the yellow (middle) row. She thought, "Does Aziz have signs in the yellow (middle) row? He has fast breathing. "The HEW classified Aziz as having pneumonia and she wrote this down on the recording room (see below).
Advise when to return immediately
Advise all mothers when to return immediately in a situation the child‘s health worsen with treatment. Tell the mother about the danger signs to bring immediately the child on treatment for pneumonia and no pneumonia.