Liver Disease
Acute Hepatitis
Acute heaptitis a disease that cause inflammation of the liver. It is usually the result of viral infection, a drug reaction, or exposure to a hepatotoxin (is a toxic /poisonous chemical substance that damages the liver). The illness represents acute hepatocellular injury with variable amounts of cell necrosis/death. Clinical manifestations generally depend both on the severity of the inflammatory reaction and, more importantly, on the amount of necrosis. Mild inflammatory reactions may present as asymptomatic elevations in the serum transaminases, whereas massive hepatic necrosis presents as acute fulminant (suddenly and with great intensity) hepatic failure. Transaminases such as serum glutamic oxaloacetic transaminases (SGOT) and serum glutamic pyruvic transaminases (SGPT) are enzymes used to synthesize and break down amino acids, normally found in the liver and heart cells which are released in the blood stream as the result of liver or heart damage, and so serve as test of liver (e.g., hepatitis)
Viral Hepatitis is most commonly due to hepatitis A, hepatitis B, or hepatitis C viruses. Patients with viral hepatitis often have a 1- to 2-week mild prodromal (An early symptom indicating the onset of an attack or a disease) illness (fatigue, malaise, low-grade fever, or nausea and vomiting) that may or may not be followed by jaundice. The jaundice typically lasts 2-12 weeks, but complete recovery, as evidenced by serum transaminases measurements, usually takes 4 months.
Drug-Induced Hepatitis can result from direct dose-dependent toxicity of a drug (or a metabolite), from an idiosyncratic drug reaction, or from a combination of the two causes. The clinical course often resembles viral hepatitis, making diagnosis difficult. Alcoholic hepatitis is probably the most commonly encountered type of drug-induced hepatitis, but the cause may not be obvious from the history.
Anesthetic Management of Patient With Acute Hepatitis
Preoperative Considerations in Acute Hepatitis
- Patients with acute hepatitis should have any elective surgery postponed until the acute hepatitis has resolved, as indicated by normalization of liver tests. Patients with hepatitis are at risk for deterioration of hepatic function and the development of complications from hepatic failure, such as encephalopathy, coagulopathy, or hepato-renal syndrome.
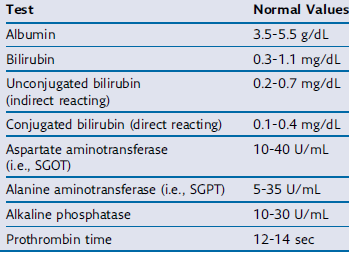
- Bilirubin and alkaline phosphatase are usually only moderately elevated. Hypoglycemia is not uncommon. Hypoalbuminemia is usually not present except in protracted cases (long duration), with severe malnutrition, or when chronic liver disease is present (Table8.1)
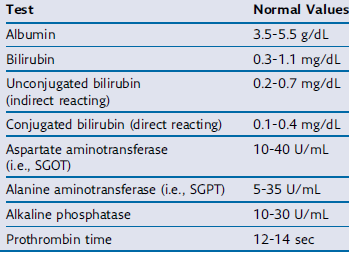
Table 8.1 Liver function test
Laboratory evaluation should include blood urea nitrogen, serum electrolytes, creatinine, glucose, transaminases, bilirubin, alkaline phosphatase, and albumin as well as a prothrombin time (PT) and platelet count. Serum should also be checked for HBsAg (hepatitis b surface antigen) whenever possible.
- If a patient with acute hepatitis must undergo an emergent operation, the preanesthetic evaluation should focus on determining the cause and the degree of hepatic impairment. Information should be obtained regarding recent drug exposures, including alcohol intake, intravenous drug use, recent transfusions, and prior anesthetics. The presence of nausea or vomiting should be noted and dehydration and electrolyte abnormalities should be corrected. Changes in mental status usually indicate severe hepatic impairment.
- Inappropriate behavior or obtundation in alcoholic patients may be signs of acute intoxication, whereas tremulousness (Marked by trembling, quivering, or shaking.) and irritability usually reflect withdrawal. Hypertension and tachycardia are often also prominent with the latter.
- Vitamin K or fresh frozen plasma (FFP) may be necessary to correct a coagulopathy. Premedication is generally not given, in an effort to minimize drug exposure and not confound hepatic encephalopathy in patients with advanced liver disease. However, benzodiazepines and thiamine are indicated for alcoholic patients with acute withdrawal.
Intraoperative Considerations in Acute Hepatitis
- The goal of intraoperative management is to preserve existing hepatic function and avoid factors that may be detrimental to the liver.
- Drug selection and dosage should be individualized. Some patients with viral hepatitis may exhibit increased central nervous system sensitivity to anesthetics, whereas alcoholic patients will often display cross-tolerance to both intravenous and volatile anesthetics. Alcoholic patients also require close cardiovascular monitoring, because the cardiac depressant effects of alcohol are additive to those of anesthetics.
- Inhalation anesthetics are generally preferable to intravenous agents because most of intravenous drugs are dependent on the liver for metabolism or elimination.
- induction doses of intravenous induction agents can generally be used causiasely. A prolonged duration of action, may be encountered with intravenous agents, particularly opioids.
- Isoflurane (if available) is the volatile agent of choice because it has the least effect on hepatic blood flow.
- Factors known to reduce hepatic blood flow, such as hypotension, excessive sympathetic activation, and high mean airway pressures during controlled ventilation, should be avoided.
- Regional anesthesia may be employed in the absence of coagulopathy, provided hypotension is avoided.
Chronic Hepatitis/Chronic Liver Disease
It is defined as persistent hepatic inflammation for longer than 6 months, as evidenced by elevated serum transaminases. Chronic liver disease involves a disease process of progressive destruction and regeneration of the liver parenchyma leading to fibrosis (formation of scar) and cirrhosis
Cirrhosis is a consequence of chronic liver disease characterized by replacement of liver tissue by fibrosis, scar tissue and regenerative nodules/lumps. It is a serious and progressive disease that eventually results in hepatic failure. Common causes include viral hepatitis B and C along with other viruses, alcohol and toxin. Manifestations are typically absent initially, but jaundice and ascites eventually develop in most patients. Other signs include spider angiomas, palmar erythema, gynecomastia, and splenomegaly. Moreover, cirrhosis is generally associated with the development of three major complications: variceal hemorrhage from portal hypertension, intractable fluid retention in the form of ascites and the hepatorenal syndrome, and hepatic encephalopathy or coma.
Anesthetic Consideration and physiological change associated with chronic liver disease
- Hematologic manifestation: Anemia, thrombocytopenia, and, less commonly, leukopenia, may be present. The cause of the anemia is usually multifactorial and includes blood loss, increased red cell destruction, bone marrow suppression, and nutritional deficiencies. Congestive splenomegaly (from portal hypertension) is largely responsible for the thrombocytopenia (law platelet count) and leukopenia (Law white blood cell count). Coagulation factor deficiencies arise as a result of decreased hepatic synthesis. Enhanced fibrinolysis (is a process that prevents blood clots from growing and becoming problematic) secondary to decreased clearance of activators of the fibrinolytic system may also contribute to the coagulopathy.
- Hyper dynamic circulation: Liver disease that has advanced to the point of cirrhosis usually results in a hyperdynamic circulation. Hemodynamic measurements generally reveal normal to low systemic blood pressure, increased cardiac output, and decreased systemic vascular resistance. Decreased systemic vascular resistance is a result of vasodilation and abnormal anatomic and physiologic shunting. Physiologic shunting is the passage of blood from the arterial to the venous side of the circulation without effectively traversing a capillary bed blood. Abnormal blood vessels, such as those seen in the skin as spider angiomas, represent an anatomic shunt.
Respiratory problems: Ascites leads to diaphragmatic splinting. Along with pleural effusions, this mechanical impairment of respiration reduces functional residual capacity and promotes atelectasis and hypoxia. Intrapulmonary arterio-venous shunting may occur, along with impaired hypoxic vasoconstriction and ventilation/perfusion (v/q) mismatching; this leads to hypoxemia and finger clubbing over time. Paracentesis (is a procedure to remove fluid that has accumulated in the abdominal cavity (peritoneal fluid)) should be considered for patients with massive ascites and pulmonary compromise but should be done with caution because removal of too much fluid can lead to circulatory collapse.
Portal hypertension: High resistance to blood flow through the liver, a hallmark of end-stage liver disease, causes an accumulation of blood in the vascular beds that are immediately upstream of the liver. Vessels draining the esophagus, stomach, spleen, and intestines dilate and hypertrophy, which leads to the development of splenomegaly and esophageal, gastric, and intra-abdominal varices (A dilated, swollen and tortuous vein that develops in veins in the linings of the esophagus and upper stomach when these veins fill with blood and swell due to an increase in blood pressure in the portal vein). Symptoms of portal hypertension include anorexia, nausea, ascites, esophageal varices, and hepatic encephalopathy. It is central to the pathogenesis of a variety of complications associated with end-stage liver disease including massive hemorrhage, increased susceptibility to infection, renal failure, and mental status changes.
Hepatic encephalopathy: Altered mental state is a frequent complication of both acute and chronic liver failure with a clinically variable presentation ranging from minor changes in brain function to deep coma. The etiology of this complex neuropsychiatric syndrome is multifactorial. Serum concentrations of a number of chemicals which are normally filtered by the healthy liver are present in higher concentrations with hepatic dysfunction, which are believed to play an important role. Ammonia is heavily implicated as a precipitating factor of episodes of hepatic encephalopathy (HE). Other etiologic factors include disruption of the blood-brain barrier, increased central nervous system inhibitory neurotransmission, and altered cerebral energy metabolism. Factors known to precipitate hepatic encephalopathy include gastrointestinal bleeding, increased dietary protein intake, hypokalemic alkalosis (from vomiting or diuresis), infections, and worsening liver function.
Impaired drug binding: When liver disease is so severe that albumin production is decreased, fewer sites are available for drug binding. This limited availability can increase levels of the unbound, pharmacologically active fraction of drugs such as thiopental. Increased drug sensitivity as a result of de creased protein binding is most likely to be manifested when plasma albumin concentrations are lower than 2.5 g/dL.
Ascites: Ascites, an accumulation of fluid in the peritoneal cavity, is a common complication of cirrhosis affecting up to 50% of cirrhotic patients. The development of ascites is associated with significant morbidity and heralds the end stages of cirrhosis. Complications associated with ascites include marked abdominal distention (leading to atelectasis and restrictive pulmonary disease), spontaneous bacterial peritonitis, and circulatory instability due to compression of the inferior vena cava and right atrium.
Although the exact mechanism of ascites is unclear, excess sodium retention by the kidney, decreased oncotic pressure due to hypoalbuminemia, and portal hypertension appear to play a central role. Initial therapy includes fluid restriction, reduction of sodium intake, and administration of diuretics. In severe cases, abdominal paracentesis can be effective at transiently reducing abdominal distention and restoring hemodynamic stability.
Renal dysfunction and hepatorenal syndrome: Renal dysfunction can develop in a significant portion of patients with cirrhosis. A variety of etiologic factors including diuretic therapy reduced intravascular volume secondary to ascites or gastrointestinal hemorrhage, nephrotoxic drugs, and sepsis can provoke acute renal failure and ultimately acute tubular necrosis in cirrhotic patients.
Liver and blood clotting: The liver helps maintain normal blood clotting in numerous ways. It is responsible for the synthesis of factors involved in coagulation (clotting), anticoagulation, and fibrinolysis (the removal of blood clots from the system by the action of fibrinolysin, an enzyme which digest fibrin.). All procoagulation factors derive from the liver, with the exception of the endothelial product, Von Willebrand factor (a protein substance involved in platelet aggregation). Precursor proteins for vitamin K-dependent coagulation are synthesized in the liver. Vitamin K catalyzes the activation of these factors (II, VII, IX, and X). Vitamin K deficiency results in the production of nonfunctional factors II, VII, IX, and X. Therefore Vitamin K should be given parenterally before 24 h for a full response.
Impact of Anesthetics on Hepatic Blood Flow
Hepatic blood flow usually decreases during regional and general anesthesia. Multiple factors are probably responsible, including both direct and indirect effects of anesthetic agents, the type of ventilation employed, and the type of surgery being performed.
All volatile anesthetic agents reduce portal hepatic blood flow. This decrease is greatest with halothane and least with isoflurane. All anesthetic agents indirectly reduce hepatic blood flow in proportion to any decrease in mean arterial blood pressure or cardiac output. Decreases in cardiac output reduce hepatic blood flow.
The hemodynamic effects of ventilation can also have a significant impact on hepatic blood flow. Controlled positive pressure ventilation with high mean airway pressures reduces venous return to the heart and decreases cardiac output. Spontaneous ventilation therefore may be more advantageous in maintaining hepatic blood flow.
Beta-Adrenergic blockers, alpha1-adrenergic agonists, H2-receptor blockers, and vasopressin reduce hepatic blood flow. Low-dose dopamine infusions may increase liver blood flow.
Perioperative Anesthetic Management of Patient With Chronic Liver Disease
- This patient should be managed with a resourceful hospital having the necessary drugs, equipment and experience to manage critically ill patient.
- You have to prepare red blood cells, fresh frozen plasma, platelets, and cryoprecipitate for management of coagulopathy and surgical blood loss.
- Patients with post necrotic cirrhosis due to hepatitis B or C who are carriers of the virus may be infectious. Extra caution is indicated in preventing contact with blood and body fluids from these patients.
- Most major operations in patients with significant liver diseases involve the use of general anesthesia. Regional techniques can be considered in selected patients with acceptable coagulation.
- The response to anesthetic agents is unpredictable in patients with cirrhosis. Changes in central nervous system sensitivity, volumes of distribution, protein binding, drug metabolism, and drug elimination are common.
- Preoperative nausea, vomiting, upper gastrointestinal bleeding, and abdominal distention due to massive ascites require a well-planned, methodical anesthetic induction. Preoxygenation and a rapid-sequence induction with cricoid pressure are most often performed. For unstable patients and those with active bleeding, either an awake intubation or a rapid-sequence induction with cricoid pressure using Ketamine (or etomidate, thiopentone in reduced dose) and succinylcholine (may have a prolonged duration of action due to reduced pseudo cholinesterase concentrations slowing its metabolism) is best advised. Cisatracurium can be used for maintenance. The dose of other long acting muscle relaxants should be reduced if used.
- The use of halothane is generally avoided so as not to confuse the diagnosis if liver tests deteriorate postoperatively. Opioids supplementation reduces the dose of other anesthetic agent required, but the half-lives of opioids are often significantly prolonged, leading to prolonged respiratory depression.
- Hypotension after induction of anesthesia occurs commonly as a result of the low systemic vascular resistance and relative hypovolemia. This can usually be treated with small doses of vasoconstrictors such as phenylephrine. With the exception of halothane, all volatile anesthetics are suitable for patients with severe liver disease. No optimal anesthetic technique has been established for the maintenance of anesthesia.
- Close respiratory and cardiovascular monitoring is necessary for patients undergoing abdominal procedures. Electrocardiographic monitoring, Pulse oximetry and blood pressure, urine catheter with other available monitor should be applied and monitored
- Judicious perioperative fluid management in patients with advanced liver disease is critical. Preoperatively, most patients are on sodium restriction, but intraoperatively preservation of intravascular volume and urinary output takes priority. The use of predominantly colloid intravenous fluids (albumin) may be preferable to avoid sodium overload and to increase oncotic pressure. Intravenous fluid replacement should take into account the excessive bleeding and fluid shifts that often occur in these patients during abdominal procedure.
Post Operative Concerns: Anesthesia and surgical interventions in patients with significant liver dysfunction precipitate decompensation. Patients with decompensated liver disease are at increased risk of postoperative hepatic failure, infection and sepsis, bleeding, poor wound healing and renal dysfunction. Benefits of critical care include ensuring optimal fluid management, renal and respiratory function monitoring, and swift correction of coagulopathy and metabolic disturbances.