Other devices that complete the equipment list, but may not be uniformly available, include: end-tidal CO2 monitoring (e.g., capnography or colorimetric device), transtracheal jet ventilation catheter, and a high-pressure oxygen source.
Laryngoscope is a tubular endoscope equipped with a blade and light bulb used to view the larynx and adjacent structures, most commonly for the purpose of inserting a tube into the trachea. Other purposes include placing a gastric tube, foreign body removal, and visualizing and assessing the upper airway. Rigid laryngoscopes commonly used in anesthesia practice are manufactured with separate detachable blade and handle. The light source is either a lamp attached to the blade or a lamp in the handle with a light guide in the blade. For a detachable handle and blade, the light source is energized when the blade and handle are locked in the operating position.
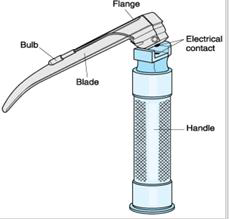
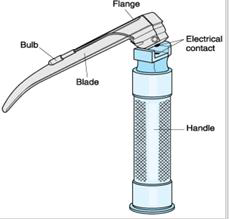
6.2.1.1 The handle of laryngoscope is the part held in the hand during use (Figure 6.1). It provides the power for the light. Most often, disposable batteries are the power source. Handles with rechargeable batteries are available. Handles designed to accept blades that have a light bulb have a metallic contact, which completes an electrical circuit when the handle and blade are in the working position.
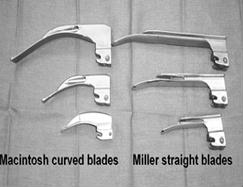
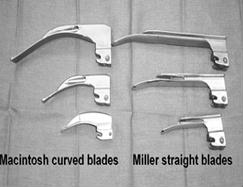
6.2.1.2 Laryngoscope blades (Figure 6.2) come in different sizes (Table 6.2). This allows for the intubation of patients of various size and age. It is important to use a blade that is appropriate for the size and age of the patient. If the blade is too small or too large it may make laryngoscopy and intubation more difficult. A straight blade is made to pick up the epiglottis commonly used in children. A curved blade is made to fit into the area anterior to the epiglottis called the vallecula. A curved blade will indirectly expose the glottic opening, by picking up the epiglottis, when you perform laryngoscopy
| Age | Straight Blade Size | Curved Blade Size |
|---|---|---|
| Newborn | 0 | |
| Infant | 0-1 | |
| Toddler 1 | 1.2 | |
| Child | 2-3 | 2 |
| Adult | 2-3 | 3-4 |
Tracheal tubes are designed to provide a secure channel through the upper airway . The distal end lies in the mid to lower part of the trachea, whereas the proximal end lies outside the mouth or nose, where it is connected to an anesthesia circuit or other device. Tracheal tubes (TT) are most commonly made from polyvinyl chloride; standards govern TT manufacturing (e.g., American National Standard for Anesthetic Equipment; ANSI Z–79) to indicate that they had been implant tested to ensure nontoxicity.
Lengths are marked in centimeters, and internal diameters are indicated in millimeters. TT size is usually designated in millimeters of internal diameter or, less commonly, in the French scale (external diameter in millimeters multiplied by 3). The choice of tube diameter is always a compromise between maximizing flow with a large size and minimizing airway trauma with a small size.
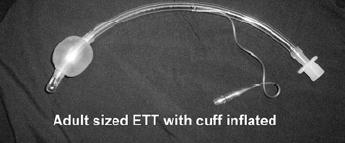
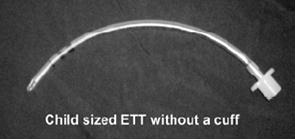
6.2.2.1 Endotracheal tube size in the adolescent and adult: An adult or adolescent female will usually require a 7.0 to 7.5 sized endotracheal tube (Figure 6.3). An adult or adolescent male will usually require a 7.5 to 8.0 sized endotracheal tube. Small adults may require a 6.0-6.5 sized endotracheal tube. Always check the cuff, ensuring it inflates and does not have a leak before insertion. When inflating the endotracheal tube cuff on adults, add just enough air to prevent an air leak. Do not over inflate the endotracheal tube cuff. This may lead to mucosal necrosis. By creating a tracheal seal, TT cuffs permit positive-pressure ventilation and reduce the likelihood of aspiration. Uncuffed tubes are usually used in children to minimize the risk of pressure injury and post-intubation croup.
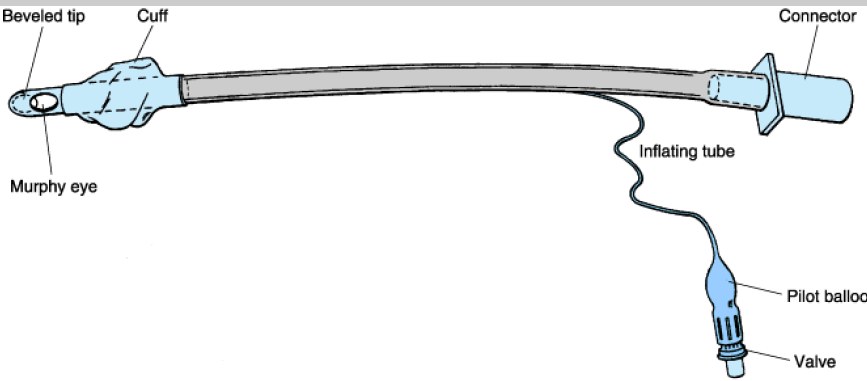
Tracheal tubes used in adult patients have a cuff near the distal end that is inflated to provide a seal against the tracheal wall to protect the lungs from pulmonary aspiration and to ensure that the tidal volume delivered ventilates the lungs rather than escapes into the upper airway. Cuffs are normally inflated with air and have an inflation tube with a pilot balloon that indicates cuff inflation.
The shape and rigidity of TTs can be altered by inserting a stylet. The patient end of the tube is beveled to aid visualization and insertion through the vocal cords. Murphy tubes have a hole (the Murphy eye) to decrease the risk of occlusion should the distal tube opening about the carina or trachea
There are two major types of cuffs: high pressure (low volume) and low pressure (high volume). High-pressure cuffs are associated with more ischemic damage to the tracheal mucosa and are less suitable for intubations of long duration. Low-pressure cuffs may increase the likelihood of sore throat (larger mucosal contact area), aspiration, spontaneous extubation, and difficult insertion (because of the floppy cuff). Nonetheless, because of their lower incidence of mucosal damage, low-pressure cuffs are more commonly recommended.
6.2.2.2 Endotracheal tube insertion depth in the adolescent and adult: The endotracheal tube should be inserted so the cuff is passed beyond the vocal cords. For most adults the depth is approximately 20-22 cm. For the small adult it may be slightly less. For the very large adult it may be slightly more.
The size of the endotracheal tube should be based on the patient's age and size. Knowledge of the differences between the adult and pediatric airway is important (Figure 6.4 A and B).
6.2.2.3Estimation of endotracheal tube size in children
6.2.2.4 Estimation of endotracheal tube insertion depth in children
Pediatric endotracheal tube recommendations
A Magill´s forceps is helpful for endotracheal tube manipulation if difficulty is encountered in positioning the endotracheal tube (Figure 6.5).
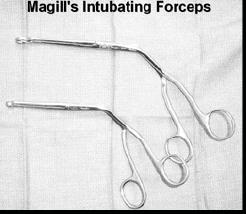 Figure 6.5 Magill’s intubating forceps Figure 6.5 Magill’s intubating forceps |
Be careful not to damage the endotracheal tube cuff with the forceps. Magill's forceps are often used to manipulate the endotracheal tube during a nasal intubation, nasogastric tube insertion and foreign body removal. |
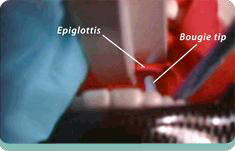
A stylet is designed to fit inside the tracheal tube and help in creating a shaped, stiff endotracheal tube (Figure 6.6). The tip of the stylet should not be allowed to protrude beyond the end of the endotracheal tube. The bougie (Figure 6.7) is flexible endotracheal tube introducer when the laryngeal opening is not fully visible (epiglottis only view) and controls the direction of the endotracheal tube during insertion. The tip of bougie should protrude through the ETT to direct the endotracheal tube through the larynx (Figure 6.8).
.png)
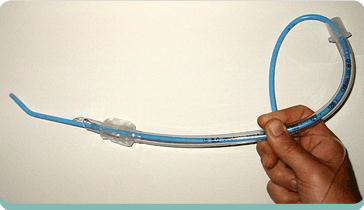
A protruding stylet may cause trauma to the patient's airway. Do not force the endotracheal tube when placing it with a stylet. This may cause trauma to your patient. The proper procedure for using a stylet is to have an assistant remove the stylet once the tip of the endotracheal tube is just past the vocal cords. Hold the endotracheal tube firmly while your assistant removes the stylet This will prevent accidental extubation of the patient. Once the stylet is removed, advance the endotracheal tube to its appropriate depth.