Continuous quality improvement is an ongoing, organization wide framework in which health service organizations and their employees are committed to and involved in monitoring and evaluating all aspects of the health service organizations‘ activities and outputs in order to continuously improve them. (American Hospital Association)
It is a continuous process with a goal of doing the right things right the first time, every time.
There are two important principles in continuous quality improvement. These are client focus and team work.
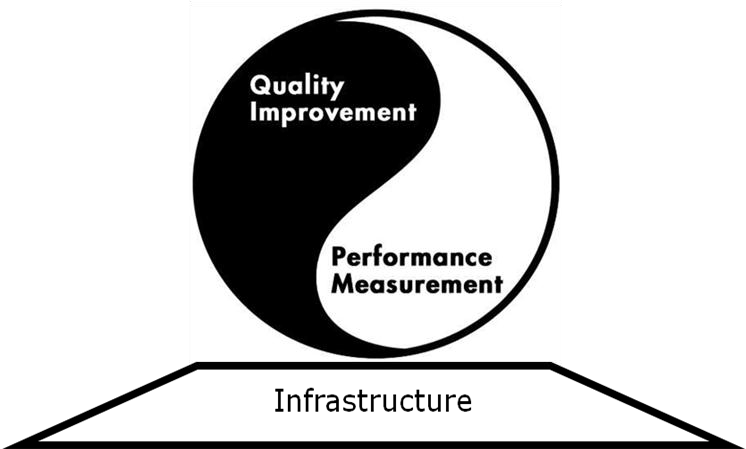
Continuous quality improvement includes two important components and a supporting infrastructure
6.4.3.1. Quality Measurement
Quality Measurement is the initial step required to initiate quality improvement processes in any kind of institution. The primary advantage of quality measurement is it helps in identifying opportunities for improvement. In addition quality management encourages improved documentation system, builds skills for analysis and interpretation of data and facilitates informed decision making in other areas.
Donabedian‘s framework for measurement of healthcare quality consist of three components measures. These are; structure, process and outcome. These quality measures are frequently confused as components of quality. Structure, process and output (S-P-O) are areas of measures on which information can be gathered and potentially inferred about the quality of healthcare.
a. Structure is the setup in which care is being provided. Structure includes:
Using structural measures as quality measures takes the assumption: If appropriate resources are available, the" likelihood of their appropriate use and then achieving attainable outcomes is high."
Eg. To measure the quality of HIV care, one can use "Percentage of hospitals with medical doctors trained on HIV care" as an indicator.
b. Process is the set of interrelated activities that constitute what healthcare is. The Assumption in process measure is "if healthcare is provided in compliance with scientific recommendations, potentially attainable outcomes will be achieved."
c. Outcome is the change observed on beneficiaries of healthcare (individuals or population) that is attributable to healthcare. It may include intermediate or longer term outcomes. Outcome measure includes: change in physical, mental and social health status, knowledge and attitude of beneficiaries and behavior/practice of beneficiaries.
How to use Structure Process and Outcome
Selection of measures depends on who will use the information. The three categories of measures are not alternatives from which someone needs to choose one. It is usually recommended to mix measures in measuring quality. While selecting measures of quality, we should consider:
Steps to measure quality
6.4.3.2. Quality Improvement
Quality Improvement is the step during which series of actions will be taken to:
The quality improvement steps are explained by the Deming‘s Cycle; which consists of four steps: Plan, Do, Study and Act
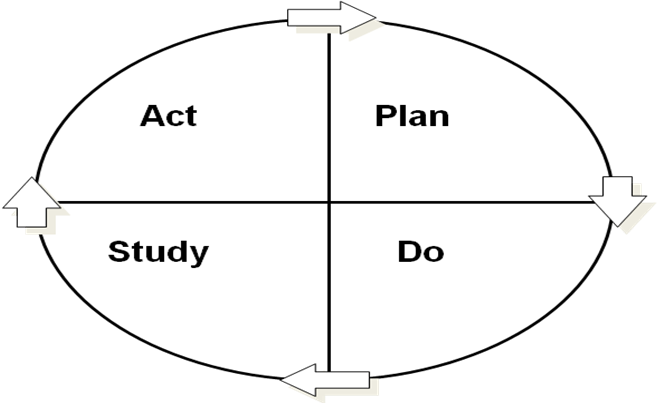
Plan
Plan -based on findings of Quality Measurement
Do
Study
– All improvements need changes but not all changes result in improvement
Act
Commonly used quality improvement actions
Quality improvement actions should be developed by considering:
Examples of actions to improve quality of healthcare:
Infrastructure is important because quality management needs to be institutionalized if improvements have to be made continually. Quality Management is not a onetime activity; always, there are rooms for improvement. It should include the human and material resources that are required to: