The bag has a tail or nipple for fresh gas flow. High concentrations of oxygen can be delivered to a mask or tracheal tube during spontaneous or controlled ventilation if a source of high fresh gas flow is connected to the inlet nipple.
Airway control is a vital component of anesthesia. Despite the best pre-operative assessment it is not always possible to foresee problems. Control of the airway is to some extent dictated by the technique used for the maintenance of anesthesia.
General anesthesia with endotracheal intubation with a cuffed tube (adult) is generally thought of as the `gold standard' for intermittent positive pressure ventilation (IPPV). The cuffed endotracheal tube is recommended in patients who are thought to have full stomach, hiatus hernia, severe oesophagitis or gross obesity, when airway access is difficult (prone position, intracranial surgery) and in prolonged surgery.
Consideration should be given about whether IPPV is more or less likely than spontaneous breathing to affect functional residual capacity (FRC) and, hence, oxygenation. If the surgical technique is likely to impair the mechanics of breathing or there is a need to secure the airway with a cuffed tracheal tube, IPPV should be employed. A patient who is already apneic from whatever cause (e.g. from drug overdose or head injury) will obviously require ventilation of their lungs.
When using intermittent positive pressure ventilation the following should adjusted on the ventilator or maintains this value when manually ventilating anesthetized patient.
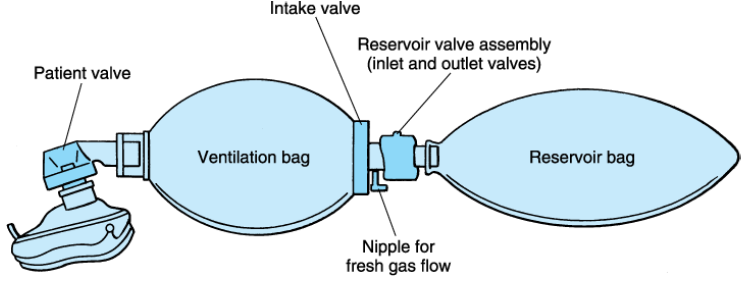
Self inflating resuscitation bag and valve apparatus attached to a mask can be used to ventilate a patient. Usually used for emergency ventilation such as, transportation of the patient, changing the empty oxygen cylinder during anesthesia and to adjust malfunction of
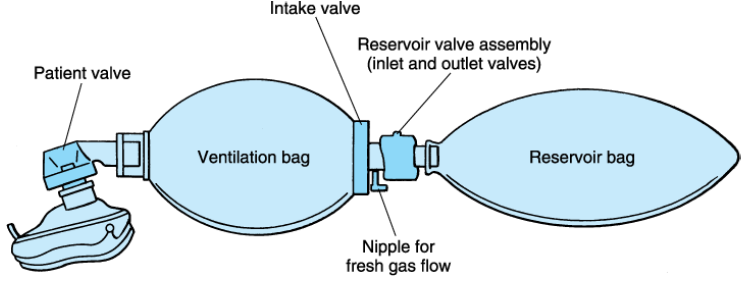
The bag has a tail or nipple for fresh gas flow. High concentrations of oxygen can be delivered to a mask or tracheal tube during spontaneous or controlled ventilation if a source of high fresh gas flow is connected to the inlet nipple.