Myocardial ischemia (coronary artery disease) is characterized by a metabolic oxygen demand that exceeds the oxygen supply. Ischemia (deficient blood supply) can therefore result from a marked increase in myocardial metabolic demand, a reduction in myocardial oxygen delivery, or a combination of both. Common causes include severe hypertension or tachycardia (particularly in the presence of ventricular hypertrophy); coronary arterial vasospasm or anatomic obstruction; severe hypotension, hypoxemia, or anemia; and severe aortic stenosis or regurgitation.
By far the most common cause of myocardial ischemia is atherosclerosis (a condition in which deposits of fats and minerals form on the walls of an artery, especially the aorta or one of the coronary or cerebral arteries, and prevent blood from flowing easily) of the coronary arteries (vessel which supply the heart muscle).
Major risk factors for coronary artery disease (CAD) include hyperlipidemia, hypertension, diabetes, cigarette smoking, increasing age, male sex, and a positive family history. Other risk factors include obesity, a history of cerebrovascular or peripheral vascular disease, menopause, use of high-estrogen oral contraceptives (in women who smoke) and a sedentary lifestyle. CAD may be clinically manifested by symptoms of myocardial necrosis (infarction), ischemia
(usually angina); arrhythmias (including sudden death), or ventricular dysfunction (congestive heart failure). Three major clinical syndromes are generally recognized: myocardial infarction (MI), unstable angina, and chronic stable angina.
Angina pectoris is typically described as retrosternal chest discomfort, pain, pressure, or heaviness. The chest discomfort often radiates to the neck, left shoulder, left arm, or jaw and occasionally to the back or down both arms. Angina may also be perceived as epigastric discomfort resembling indigestion. Some patients describe angina as shortness of breath, mistaking a sense of chest constriction as dyspnea. The need to take a deep breath, rather than to breathe rapidly, often identifies shortness of breath as an anginal equivalent. Physical exertion, emotional tension, and cold weather may induce angina; rest and/or nitroglycerin relieve it.
3.1.2.2 Chronic stable angina refers to chest pain or discomfort that does not change appreciably in frequency or severity over 2 months or longer. Unstable angina is defined as an abrupt increase in severity, frequency (more than three episodes per day), angina at rest, or new onset of angina (within the past 2 months) with severe or frequent episodes (more than three per day). The anginal episodes are often not related to any apparent precipitating factors. Unstable angina may also occur following MI or be precipitated by noncardiac medical conditions (including severe anemia, fever, infections, thyrotoxicosis, hypoxemia, and emotional distress) in previously stable patients.
Unstable angina, particularly when it is associated with significant ST-segment changes at rest, usually reflects severe underlying coronary disease and frequently precedes MI. Plaque disruption with platelet aggregates or thrombi and vasospasm are frequent pathological correlates. Critical stenosis in one or more major coronary arteries is present in over 80% of patients. Patients with unstable angina require cardiologist/ internist evaluation urgent evaluation and treatment. Anticoagulation with heparin is usually instituted, together with aspirin, intravenous nitroglycerin, -blockers, and, possibly, calcium channel blockers.
3.1.2.3 Acute myocardial infarction (AMI) serious complication of ischemic heart disease results in sudden death of part of myocardium from ischemia and necrosis of part of the myocardium. It is felt as a sense of heavy pressure or squeezing pain in the chest, often radiating to the shoulder and arm. Infarctions weaken the heart wall and disrupt electrical conduction pathways, potentially leading to fibrillation and cardiac arrest. The immediate treatment of AMI is the administration of oxygen (4–6 L/min), aspirin (160–325 mg), nitroglycerin (sublingual or spray), and morphine (2–4 mg intravenously every 5 min) until the pain is relieved. Remember the acronym: MONA (morphine, oxygen, nitroglycerin, and aspirin) greets all patients.
The general approach in treating patients with ischemic heart disease is 5-fold:
3.1.2.4 Optimization of the myocardial ischemic patient by the internist/ cardiologist
Patient with a known heart disease including ischemic heart disease shall be referred to a resourceful hospital that could handle cardiac patients. Preventing ischemic heart disease under anesthesia is a vital importance at any level of hospital. Only if your patient needs emergency surgery and could not be referred consider the following:
The same general principles that apply to patients with hypertension also apply to most patients with ischemic heart disease. Management of anesthesia should balance between myocardial oxygen requirements and myocardial oxygen delivery to prevent myocardial ischemia. Persistent tachycardia, systolic hypertension, arterial hypoxemia, or diastolic hypotension can adversely influence this delicate balance. Persistent and excessive changes in heart rate and systemic blood pressure should be minimized. Maintaining heart rate and systemic blood pressure within 20% of the awake values is commonly recommended.
3.1.3.1 Preanesthetic consideration:
History: The preoperative history is meant to elicit the severity, progression, and functional limitations imposed by ischemic heart disease. Questions should encompass symptoms, current and past treatment, complications, and the results of previous evaluations. This information will provide some estimate of disease severity and heart function. The most important symptoms to elicit include chest pains, dyspnea, poor exercise tolerance and syncope. The relationship between symptoms and activity level should be established. Activity should be described in terms of everyday tasks such as walking or climbing stairs. Cough, cigarette smoking, renal disease, diabetes mellitus and other systemic disease should be looked. It is common practice to delay elective surgery for some time at least 6 weeks following an acute myocardial infarction.
Current medications: Drugs most likely taken by patients with coronary artery disease are beta-adrenergic antagonists, nitrates, calcium channel blockers, angiotensin-converting enzyme inhibitors, drugs that decrease blood lipids, diuretics, antihypertensive, and platelet inhibitors (Asprin). A potential adverse interaction of these drugs with anesthetics is an important preoperative consideration. β-blocker therapy should be continued throughout the perioperative period. Atropine or glycopyrrolate can be used to treat excessive chronotropic effects of β- blockers during the perioperative period. Many recommend withholding ACE inhibitors for 24 hours before surgical procedures involving significant fluid shifts or blood loss.
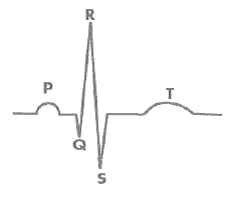
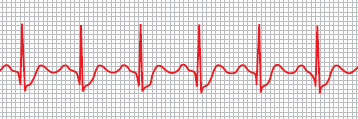
Electrocardiograph: The preoperative ECG should be examined for evidence of myocardial ischemia and prior myocardial infarction. The exercise ECG simulates sympathetic nervous system stimulation as may accompany perioperative events such as direct laryngoscopy, tracheal intubation, and surgical incision. The resting ECG in the absence of angina pectoris may be normal despite extensive coronary artery disease (Figure 3.1). An ECG demonstrating ST-segment depression confirms the presence of myocardial ischemia (Figure3:2).
Laboratory evaluation: Hematocrits less than 28% have been associated with perioperative ischemia and postoperative complications, particularly in patients who has large blood loss.
3.1.3.5 Maintenance of anesthesia
3.1.3.6 Muscle Relaxants: The choice of nondepolarizing neuromuscular blocking drug during maintenance of anesthesia for patients with coronary artery disease may be influenced by the circulatory effects of these drugs. Vecuronium, rocuronium, and cisatracurium do not evoke histamine release and associated decreases in systemic blood pressure, even with the rapid intravenous administration of large doses. Likewise, the systemic blood pressure lowering effects of atracurium are usually modest, especially if the drug is injected over 30 to 45 seconds to minimize the likelihood of drug-induced histamine release. Pancuronium increases heart rate and systemic blood pressure, but these changes are usually less than 15% above pre-drug values. Use of pancuronium has decreased with the increased use of more selective neuromuscular blocking drugs (vecuronium, rocuronium, and cisatracurium). Nondepolarizing neuromuscular blockade in patients with coronary artery disease can be safely antagonized with anticholinesterase drugs combined with an anticholinergic drug. Glycopyrrolate has more titratable chronotropic effects than atropine.
3.1.3.7 Post operative care: Recovery from anesthesia and the immediate postoperative period can continue to stress the myocardium. The patient should receive supplemental oxygen until adequate oxygenation is established. Shivering usually resolves following administration of meperidine, 20–30 mg intravenously. Hypothermia should be corrected with a forced-air surface warmer. Postoperative pain should be controlled with generous analgesics. If there is a suspicion of fluid overload or the patient has a history of poor ventricular function, a postoperative chest film is useful. Pulmonary edema can be rapidly treated with furosemide, 20–40 mg intravenously. The greatest risk to these patients postoperatively is unrecognized ischemia.