4.2 Specific respiratory problems: URI & Asthma
4.2.1 Upper respiratory infection:
4.2.1.1 Upper respiratory infection (URI) is a term for almost for any kind of infectious disease process involving the nasal passages, pharynx, and bronchi. Common cold or mild upper respiratory infection occurs once or twice a year in adults. In children the incidence is more frequent occurring once in two months. Because of the very frequent incidence in children, it is difficult to find upper respiratory free period for elective surgeries. The etiological agent may be bacterial or viral and is rarely accurately known. Patients with upper respiratory infection present broad spectrum of signs and symptoms including sneezing, runny nose, and a history of allergies. When associated with infection, fever, purulent nasal discharge, productive cough, and malaise can be seen.
The viral infection of the respiratory tract causes inflammation and edema of the nose, throat and lower airways. This causes airway obstruction and increased airway reactivity and is responsible for the cough, laryngo and bronchospasm. One mm edema causes just a marginal increase in the airway resistance in adults, but in infants with narrow trachea, this may lead to 75% reduction in the airway causing serious airway obstruction. This is the main reason why infants desaturate faster than children and URI exacerbated this problem.
4.2.1.2 Anesthetic management: A patient might be seen several days before surgery without any contraindication to the upcoming procedure. However, on the day of surgery, the patient may have an upper respiratory infection (URI). Consultation with the surgeon regarding the urgency of the case must be undertaken. The economic and practical aspects of canceling surgery should be taken into consideration before a decision is made to postpone surgery. If the child is presenting for an emergent procedure, the presence of URI should be elicited if possible, because this knowledge will alert the anesthetist to the potential for complications and may permit modification of the anesthetic management to reduce any risk. Children presenting for elective procedures with symptoms of a URI require careful preoperative assessment, including a detailed history and physical examination.
In adult, acute upper and lower respiratory infection by itself or exacerbated chronic chest infections such as chronic bronchitis which is characterized by dyspnea and chronic cough with sputum need preoperative management to reduce the volume of sputum by chest physiotherapy and postural drainage, advice not smoke for at least 48 hours before the operation if possible for 15 days. If there is any evidence of infective process, e.g. yellow sputum, fever; test the sputum by culture and sensitivity if the facilities are available and use the appropriate antibiotic. Elective surgery should be postponed.
4.2.1.2.1 Preanesthetic assessment: Consider the preoperative preparation of patient for respiratory diseases
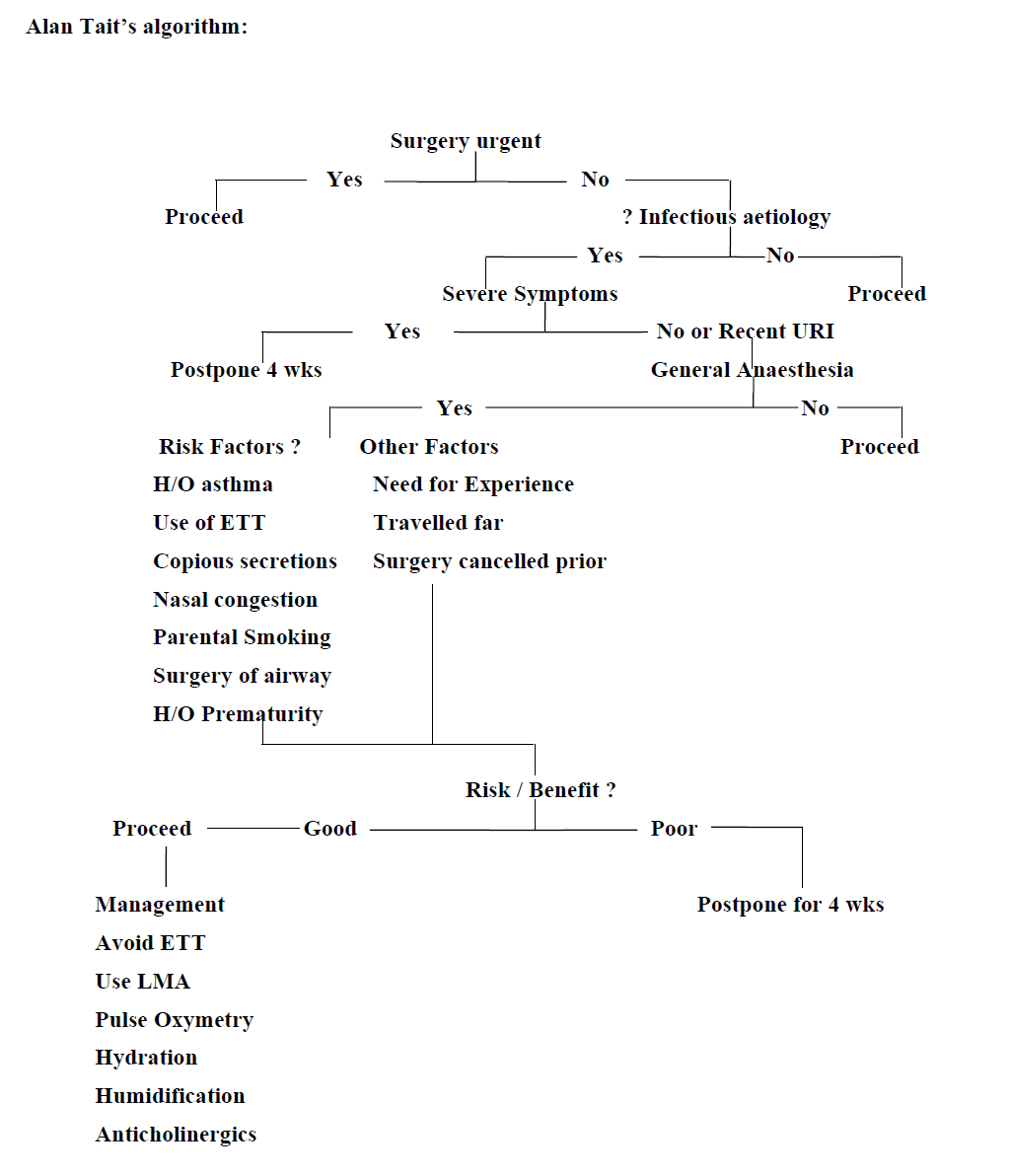
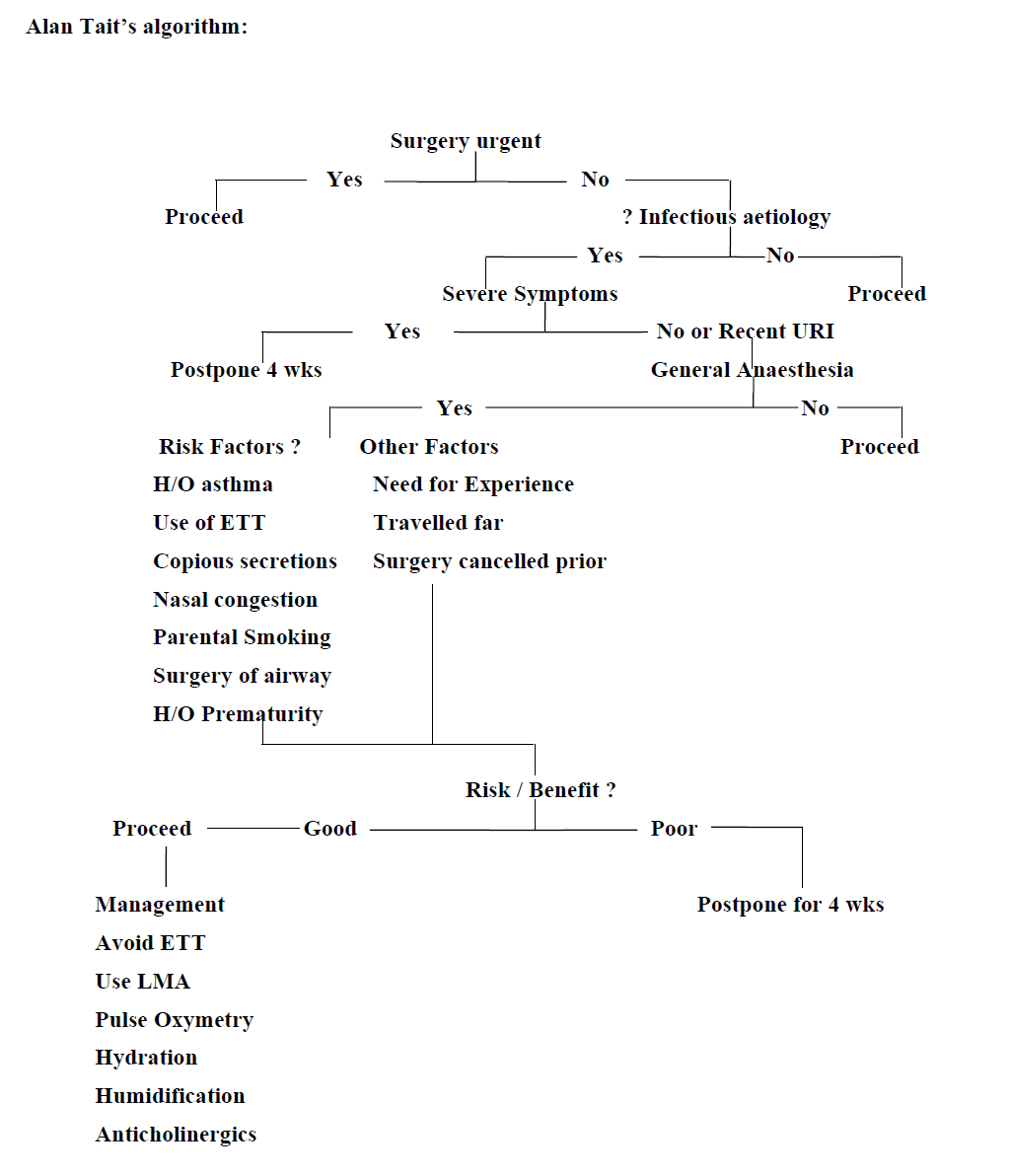
- In assessing the suitability of any child with a URI for surgery, it is important to assess the risk/benefit ratio (Table4.2). This should involve consideration of the child’s presenting symptoms and age, the urgency of the surgery, comorbid conditions (e.g., asthma or cardiac disease), and the type of surgery. Another consideration is the frequency of URIs experienced by the child. In the case of the child who experiences six to eight URIs per year, it may be difficult to precisely target a period when the child is symptom free for elective surgery.
- The patient should be evaluated for fever, dyspnea, productive cough, sputum production, nasal congestion, lethargy, and wheezing. Nasal congestion, sputum production, and a history of reactive airway disease are predictors of adverse respiratory events.
- The lungs should be auscultated to exclude any lower respiratory tract involvement, and a chest radiograph (if possible) should be considered if the examination is questionable. At this point the surgeon or other medical specialist can assist you in establishing the diagnosis and initiate management.
- In general, children presenting with symptoms of an uncomplicated URI and who are afebrile with clear secretions and appear otherwise healthy, or those with noninfectious conditions, should be able to undergo surgery; if you have the experience, the necessary anesthetic agents and adjunct to manage this specific patient.
- Children with more severe symptoms including mucopurulent secretions, productive cough, fever -38°C, lethargy, or signs of pulmonary involvement should have their elective surgery postponed for a minimum of 4 weeks and should be placed on antibiotic therapy.
4.2.1.2.2 Intraoperative anesthetic management of patients with URI (table 4:2)
- If possible, in adult spinal anesthesia for lower abdominal and lower extremity procedures
- If the procedure is emergency and require endotracheal tube insertion consider the anesthetic management for emergency patient – rapid sequence induction.
- Management of the child with a URI is directed at minimizing secretions, minimizing airway manipulation time and avoiding stimulation of a potentially sensitive airway. Because sputum and copious secretions have been identified as risk factors, it is important that the airway be suctioned (under deep anesthesia) to remove excess secretions. This not only reduces airway irritation from secretions, but also may be important in preventing mucus from plugging abronchus or endotracheal tube.
- Airway reflexes are heightened in patients with URI and in those with recent history of URI. This hypersensitivity is highest in the first three days of URI, though persisting for two to three weeks to a lesser degree. In adult patients with bronchial hyper-reactivity, preoperative treatment with combined corticosteroids and salbutamol minimized intubation-evoked bronchoconstriction more effectively than inhaled salbutamol alone.
- Nebulized (Nebulizer is an instrument which sprays liquid in the form of very small drops like mist) lidocaine attenuated the heightened airway reflex sensitivity associated with symptoms and signs of upper respiratory tract infection or try lidocaine with out adrenaline and preservative 1mg/kg intravenously.
- Patients should be adequately hydrated and humidification of the anaesthetic gases should be employed to avoid thickenning of respiratory secretions. IV hydration should be instituted in all patients unless the procedure is very short. Humidification may also be important in children with URIs, particularly for long cases.
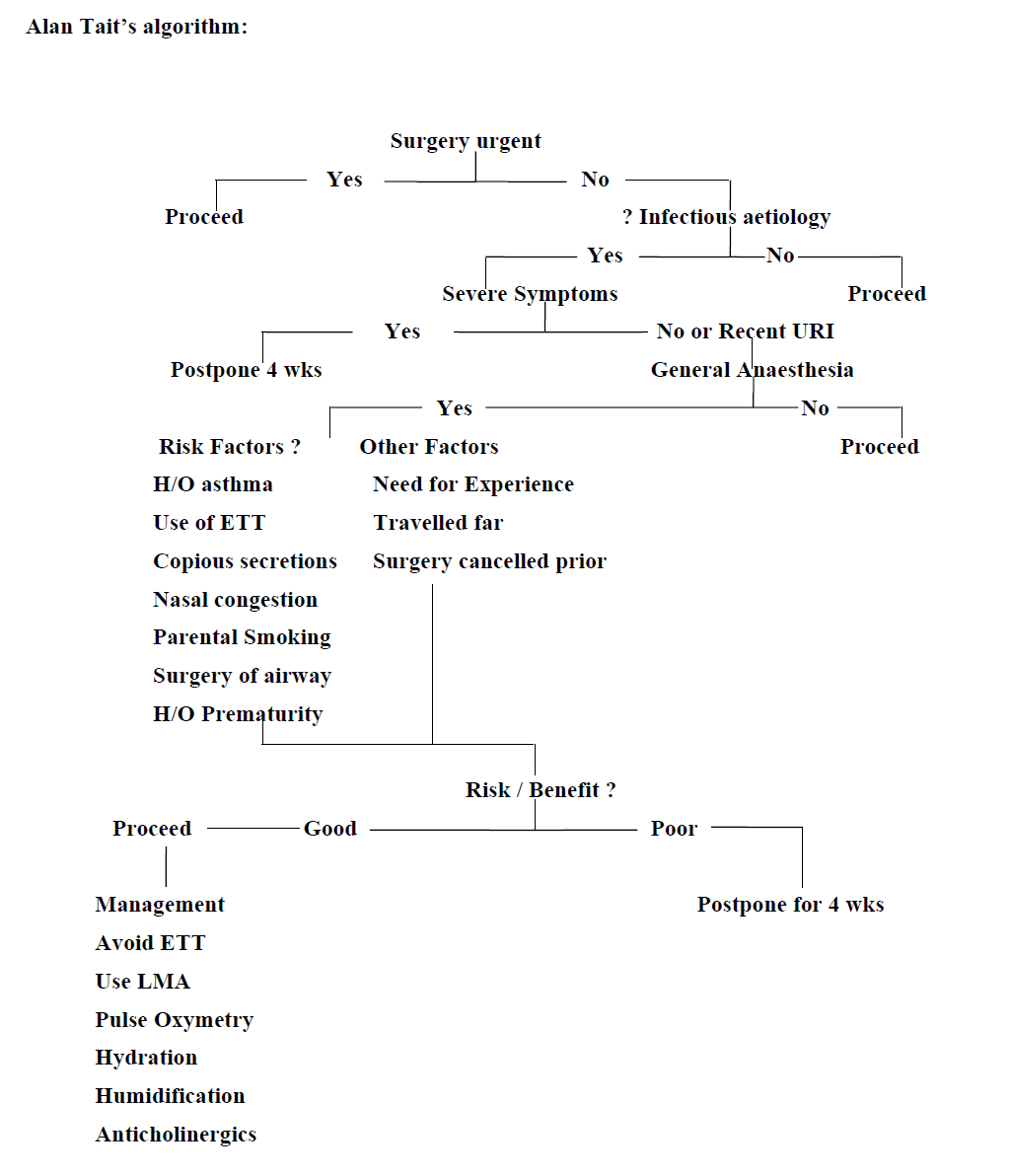
Table 4:2 Algorithm of anesthetic management for a patient upper respiratory infection
- Use of an endotracheal tube (ETT) should be avoided if possible, because its use, particularly in young children, significantly increases the risk of airway complications. Although a face mask is associated with the least incidence of complications, it may not be appropriate for certain cases. For example, an ETT is likely the airway of choice for surgery of the oropharynx and neck, abdominal surgery, and operations lasting more than a couple of hours. The LMA, however, has been shown to provide a safe alternative for some procedures in which an ETT might otherwise be used.
- If intubation is mandatory, it is preferable to give atropine premedication and salbutamol nebulisation in the preoperative period.
- The choice of anesthetic for induction and maintenance has been shown to be important in children with URIs. Halothane because we donot have sevoflurane is prefered for smoother inhalation induction which is less likely to depress respiratory system. Ketamine should preced by anticholinergics to reduce secretion.
- The tracheobronchial trees should be suctioned well before extubation (under deep anesthesia)
- In any case, all patients should be monitored continuously by pulse oximetry, particularly during the placement and removal of an ETT and in the immediate postoperative period.
- Regardless of the induction drug used, it is imperative that the depth of anesthesia be sufficient to obtund the airway reflexes, particularly when an ETT is placed. Some anesthetist prefer to extubate under deep anesthesia to avoid reflex constriction of the airways, others prefer to extubate when the patient is awake, believing that a patient with intact reflexes is in a better position to clear secretions and respond to the tactile stimulation of ETT removal.
- Long-term complications from anesthetizing patients with URI have not been demonstrated. Intraoperative and immediate postoperative hypoxemia is common and amenable to treatment with supplemental oxygen.
4.2.2 Anesthetic management for asthmatic patient
4.2.2.1 Asthma
Asthma is a disease characterized by chronic airway inflammation, reversible expiratory airflow obstruction in response to various stimuli, and bronchial hyper reactivity. Airway hyper- responsiveness may result in the development of bronchoconstriction in response to stimuli (allergens, exercise, and mechanical airway stimulation) that have little or no effect on normal airways. The classic symptoms associated with asthma are cough, shortness of breath, and wheezing. The intensity of these symptoms is variable, ranging from cough with or without sputum production to chest pain, tightness and dyspnea. High-pitched, musical wheezes during expiration are characteristic of asthma, although they are not specific. Elimination of obstruction after the administration of a bronchodilator drug suggests a diagnosis of asthma. Classically, the obstruction is precipitated by a variety of airborne substances, including pollens, animal danders, dusts, pollutants, and various chemicals. Exercise, emotional excitement, and viral infections also precipitate bronchospasm in many patients.
Drug therapy in asthma: Mild asthma is usually treated intermittently with an inhaled beta agonist such as salbutamol to control symptoms. When this provides insufficient control, a regular inhaled steroid such as beclomethasone is added. In order to gain maximally from the anti-inflammatory action, steroid needs to be taken regularly. By using inhaled steroids, long term systemic side effects of steroids are minimized. Patients who are not controlled by this regime are usually treated with a number of second line drugs including salmeterol (long acting beta agonist which must be used with an inhaled steroid), ipratropium (anticholinergic), aminophylline, and oral steroids. In acute episodes, oral prednisolone taken for 7 – 10 days is often effective.
Table 4:3 Management of severe bronchospasm outside of theatre:
Start high flow oxygen and gain IV access. According to facilities try:
- Nebulized salbutamol (if available) 5 mg. May be given continuously at 5–10 mg/hour. An alternative is a metered dose inhaler. 5-10 puffs should be given initially.
- IV salbutamol if not responding (250 mcg slow bolus then 5–20 mcg/min).
- Hydrocortisone 100 mg IV 6 hourly or prednisolone orally 40–50 mg/day.
- Magnesium 2g IV over 20 minutes
- Aminophylline 5mg/kg IV followed by infusion may be effective.
- In extremis (decreasing conscious level or exhaustion) adrenaline may be used: nebulizer .5 ml of 1 in 1,000 with 3 ml of saline; IV 10 mcg (0.1 ml 1: 10,000) increasing to 100 mcg (1 ml 1: 10,000) depending on response. Beware arrhythmias in the presence of hypoxia and hypercapnia. If intravenous access is not available subcutaneous or intramuscular administration (0.5–1 mg) may be used, though absorption may be unpredictable due to poor perfusion.
4.2.2.2 Anesthetic management for bronchial asthma: Elective surgery should take place when the patient’s asthma is optimally controlled. Most well-controlled asthmatics tolerate anesthesia and surgery well. The frequency of complications is increased in patients over 50 years, those undergoing major surgery and in those with unstable disease. Poorly controlled asthmatics (those with current symptoms, frequent exacerbations or hospital admissions) are at risk of perioperative respiratory problems (bronchospasm, sputum retention, atelectasis, infection and respiratory failure).
4.2.2.2.1Preoperative assessment: Patients are best able to be assessed their current asthma control. In chronic disease, patients and doctors frequently underestimate the severity of asthma.
- Ask about exercise tolerance (e.g. breathless when climbing stairs, walking on level ground, or when undressing) and general activity levels. Complete resolution of recent exacerbations should be confirmed by chest auscultation. No wheezing, no dyspnea and no cough
- Clearly document any allergies or drug sensitivities, especially the effect of aspirin or other non-steroidal anti-inflammatory drug (NSAIDs) on asthma. The prevalence of aspirin (or other NSAID) induced asthma is 21% in adult asthmatics, and 5% in pediatric asthmatics.
- Asthmatic patients with active bronchospasm presenting for emergency surgery should be treated aggressively whenever possible. Supplemental oxygen, aerosolized β 2-agonists, and intravenous glucocorticoids can dramatically improve lung function in a few hours.
- Viral infections are potent triggers of asthma, so postpone elective surgery if symptoms suggest URI.
- Some degree of preoperative sedation is desirable in asthmatic patients presenting for elective surgery particularly in patients whose disease has an emotional component. In general, benzodiazepine (diazepam 5- 10 mg IV) is the most satisfactory agents for premedication.
- Anticholinergic agents are not customarily given unless very copious secretions are present or if ketamine is to be used for induction of anesthesia. In typical intramuscular doses, anticholinergics are not effective in preventing reflex bronchospasm following intubation.
- Bronchodilators should be continued up to the time of surgery.
- Patients who have been receiving long-term glucocorticoid therapy should be given supplemental doses to compensate for adrenal suppression. Hydrocortisone (50–100 mg preoperatively and 100 mg every 8 h for 1–3 postoperative days, depending on the degree of surgical stress) is most commonly used.
4.2.2.2.2 Intraoperative management
- Patients with mild and well-controlled asthma can be safely anesthetized with any technique, as long as airway irritation is minimized. For example, general anesthesia through a face mask and laryngeal mask airway is less stimulating to the airway than through an endotracheal tube. When asthma is poorly controlled, regional techniques are ideal for peripheral and lower abdominal surgery.
- If general anesthesia is chosen, additional inhaled bronchodilator therapy immediately prior to induction of anesthesia is effective in blunting the onset of bronchospasm. Regional anesthesia, when applicable, should always be considered in the severely asthmatic patient. Ask the patient to take 2 puffs from their prescribed salbutamol inhaler 30 minutes before surgery.
- The goal of any general anesthetic is a smooth induction and emergence, with anesthetic depth adjusted to stimulation. The most critical time for asthmatic patients undergoing anesthesia is during instrumentation of the airway. A sufficient depth of anesthesia should be established before tracheal intubation.
- Induction agent is chosen to achieve deep anesthesia before intubation and surgical stimulation. Ketamine has a bronchodilation effect and its increasing secretion effect should be blunted by atropine or glycopyrrolate. These anticholinergic drugs have also a bronchodilation effect. Propofol and etomidate are suitable alternatives. Thiopental is most commonly used for adults but occasionally can induce bronchospasm. Halothane usually provides the smoothest inhalation induction with bronchodilation in asthmatic children as well as in adult.
- Administration of 1-2 mg/kg of lidocaine blunt reflex bronchospasm. All opiates blunt airway reflexes and can be helpful during the induction of general anesthesia. Muscle relaxants, often recommended during severe acute bronchospasm, do not affect smooth musculature, and their alleged utility is likely related to the facilitation of mechanical ventilation that occurs with relaxation of the skeletal musculature of the chest wall. Both opiates (morphine) and some muscle relaxants may cause bronchospasm through the release of histamine
- Controlled ventilation with the use of neuromuscular blocking drugs will be needed for major or long procedures. In cases with severe airways obstruction the ventilator rate may have to be sufficiently low to allow the slow expiration of asthma.
- At the completion of surgery, the patient should ideally be free of wheezing. Reversal of nondepolarizing neuromuscular blocking agents with anticholinesterase agents does not precipitate bronchoconstriction if preceded by the appropriate dose of an anticholinergic (Atropine).
- Deep extubation (before airway reflexes return) prevents bronchospasm on emergence. Lidocaine as a bolus (1–2 mg/kg) may help obtund airway reflexes during emergence. For a patient at increased risk for aspiration of gastric content extubation shall be awake.
4.2.2.2.3 Postoperative care
- Pain relief is important particularly following major abdominal or thoracic surgery. Regular administration of opioids is the most common technique. Pethidine may be more appropriate than morphine if there has been morphine associated bronchospasm in the past.
- Avoid aspirin and any other allergens known to the patient.
- Oxygen can be administered until the patient maintains his/her saturation with atmospheric air.
- Maintenance of hydration with intravenous fluids is required until oral intake is sufficient.
- Usual anti-asthmatic medications are resumed immediately.