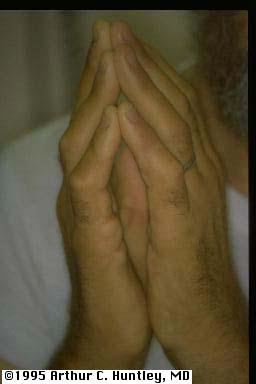
To test if a patient is at risk, ask them to bring their hands together, as if praying, and simultaneously hyperextend to 90 degrees at the wrist joint. If the little fingers do not oppose, anticipate difficulty in intubation.
Many of the operations diabetic patients face are a direct result of their disease. Skin ulcers, amputations and abscesses are amongst the commonest. Successful management of the diabetic patient depends as much, if not more, on the proper management of the chronic complications of the disease as on acute glycemic management.
A thorough preoperative search must be done for end-organ complications of diabetes mellitus. In addition to a thorough history and physical, a recent ECG, blood urea nitrogen, potassium, creatinine, glucose, and urinalysis are essential.
5.3.1.1 Anesthetic consideration of symptoms of secondary involvement of other organs: Diabetes causes disease in many organ systems, the severity of which may be related to how long the disease has been present and how well it has been controlled.
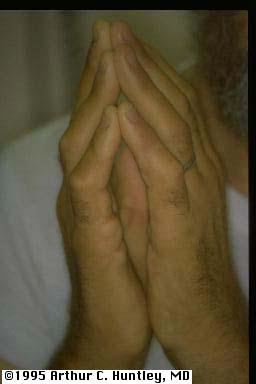
To test if a patient is at risk, ask them to bring their hands together, as if praying, and simultaneously hyperextend to 90 degrees at the wrist joint. If the little fingers do not oppose, anticipate difficulty in intubation.
The primary goal of intraoperative blood sugar management is to avoid hypoglycemia. Unacceptably loose blood sugar control (> 180 mg/dL) also carries risk. Hyperglycemia has been associated with hyperosmolarity (dehydration), infection, and poor wound healing. There are several perioperative management regimens for diabetic patients.
5.3.2.1 Alternative regimen 1: In the most common, the patient receives a fraction usually half of the total morning insulin dose in the form of intermediate-acting insulin. To decrease the risk of hypoglycemia, insulin is administered after intravenous access has been established and the morning blood glucose level is checked. For example, a patient who normally takes 30 U of NPH (neutral protamine Hagedorn; intermediate-acting) insulin and 10 U of regular or Lispro (short-acting) insulin or insulin analogue each morning and whose blood sugar is at least 150 mg/dL would receive 15 U (half of 30, half the normal morning dose) of NPH subcutaneously or intramuscularly before surgery along with an infusion of 5% dextrose solution (1.5 mL/kg/h). Absorption of subcutaneous or intramuscular insulin depends on tissue blood flow
Dedication of a small-gauge intravenous line for the dextrose infusion prevents interference with other intraoperative fluids and drugs. Supplemental dextrose can be administered if the patient becomes hypoglycemic (< 100 mg/dL). However, intraoperative hyperglycemia (> 150–180 mg/dL) is treated with intravenous regular insulin according to a sliding scale. One unit of regular insulin given to an adult usually lowers plasma glucose by 25–30 mg/dL.
5.3.2.2 Alternative regimen 2
Steps to select appropriate management regime
1. Decide on the type of surgery
2. Then, is the patient insulin or non-insulin dependent?
3. Finally :
General Measures for all diabetics: Measure random sugar preoperatively - 4 hourly for IDDM & 8 hourly for NIDDM
If the patient is taking an oral hypoglycemic agent preoperatively instead of insulin, the drug can be continued until the day of surgery, but sulfonylureas and metformin should not be used for 24–48 h before surgery because of their long half-lives. They can be started postoperatively when the patient is taking drugs per os. Metformin is restarted if renal and hepatic functions remain adequate. Because of the long duration of action, a glucose infusion is begun and blood sugars are monitored as though intermediate-acting insulin had been given.
| Non insulin Dependent
Diabetics
Note 1mmol/l = 18mg/dl |
Preoperatively - random blood sugar
On admission - < 10 mmol/l Normal medication until day of op > 10 mmol/l Follow as for MAJOR SURGERY Day of operation Omit oral hypoglycemic Blood glucose- 1 hour preop and at least once during op (hourly if op > 1 hour long) postop - 2 hourly until eating then 8 hourly Postoperatively Restart oral hypoglycemics with first meal |
| Insulin dependent
Diabetics This regime only suitable for patients whose random sugar is < 10 mmol/l on admission, will only miss one meal preoperatively & are first on the list for very minor surgery eg cystoscopy |
Preoperatively: Normal medication
Day of operation: No breakfast, no insulin, place first on list. Blood glucose- 1 hour preoperatively and at least once during op (hourly if op > 1 hour long) postoperatively - 2 hourly until eating then 4 hourly Postoperatively: Restart normal subcutaneous insulin regime with first meal |
Day of operation
Regime 1 - no infusion pump available. Start intravenous infusion of 5 or10 % dextrose (500 ml bags) over 4 - 6 hours and add Insulin and Potassium. Chloride (KCl) to each 500 ml bag as below. Change bag according to blood sugar level readings:
| Blood glucose (mmol/l) |
Soluble insulin(units)
to be added to bag |
Blood potassium (mmol/l) |
KCl(mmol) (to be added to bag) |
|---|---|---|---|
| 4 | No insulin | ||
| 4 - 6 | 5 | < 3 | 20 |
| 6-10 | 10 | 3-5 | 10 |
| 10-20 | 15 | >5 | None |
| >20 | 20 |
If blood potassium level not available, add 10 mmol KCl
Postoperatively:
Non-insulin dependent
Insulin dependent
Remember that the patient may need additional fluids depending on surgery, blood loss etc.