Mothers who are HIV-positive and their babies need special care before, during and after labour and delivery. Therefore, if the mother is counselled and HIV-tested before or during pregnancy, and she knows that she is HIV positive, you should try to convince her to deliver her baby in a health facility. That way she and her baby will get special care from health professionals with special training in delivering babies from HIV-positive mothers, and prevent maternal to child transmission (PMTCT of HIV).
In the postnatal period, she may need to take antiretroviral (ARV) drugs prescribed for her by the HIV clinic, and your support is vital in helping her to keep to her drug regimen.
Maintain confidentiality about her status and conduct frequent visits to this woman as she may require a lot of psychosocial support immediately after the delivery. If it is available link her with the community social support group. Always make sure her partner is counselled and HIV-tested and also involved in the whole care process.
In this study session, our focus is on the risk of HIV being transmitted from the mother to her newborn baby in her breast milk, and how you can support and counsel her about feeding options. If 20 HIV-positive mothers breastfeed their HIV-negative babies exclusively for the first six months, on average one to three of the babies will become infected with HIV through its mother's breast milk.
So the mother has a difficult choice to make. She has to balance the risk to her baby from HIV transmission during breastfeeding, against the risk of not breastfeeding and losing all the benefits described above. Formula feeding also exposes the baby to increased risk of infection from unsterilized bottles and malnutrition from incorrectly made feeds.
Exclusive breastfeeding is NOT recommended for the babies of HIV-positive women since the only way to protect the baby completely from HIV transmission from its mother is to feed it on formula milk. This is known as replacement feeding. However, many families cannot afford to buy milk formula to feed the baby, and bottle feeding may be socially unacceptable in some communities.
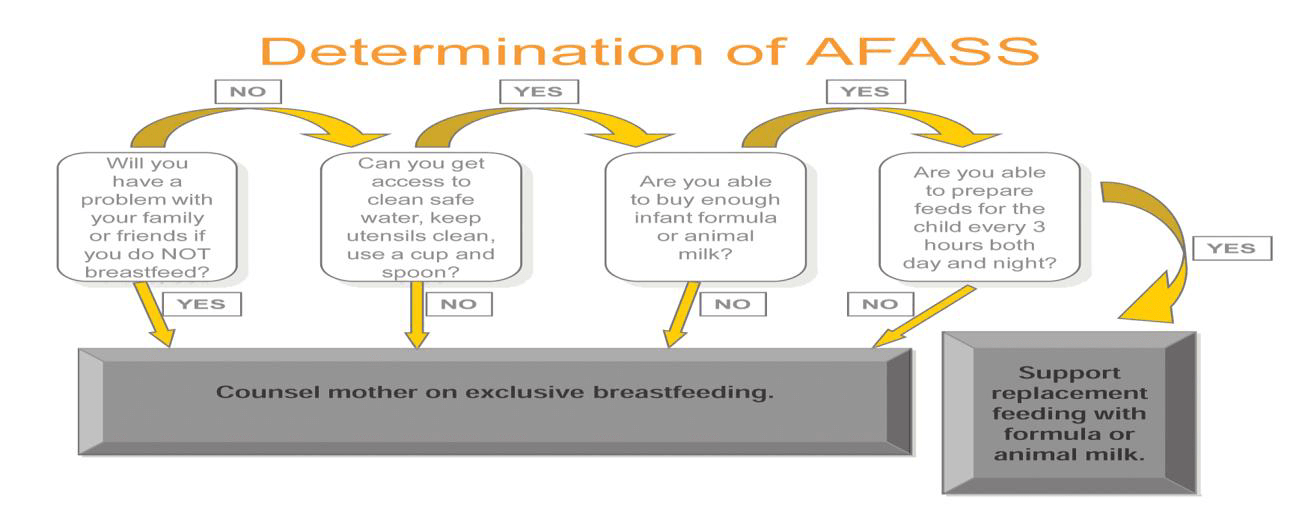
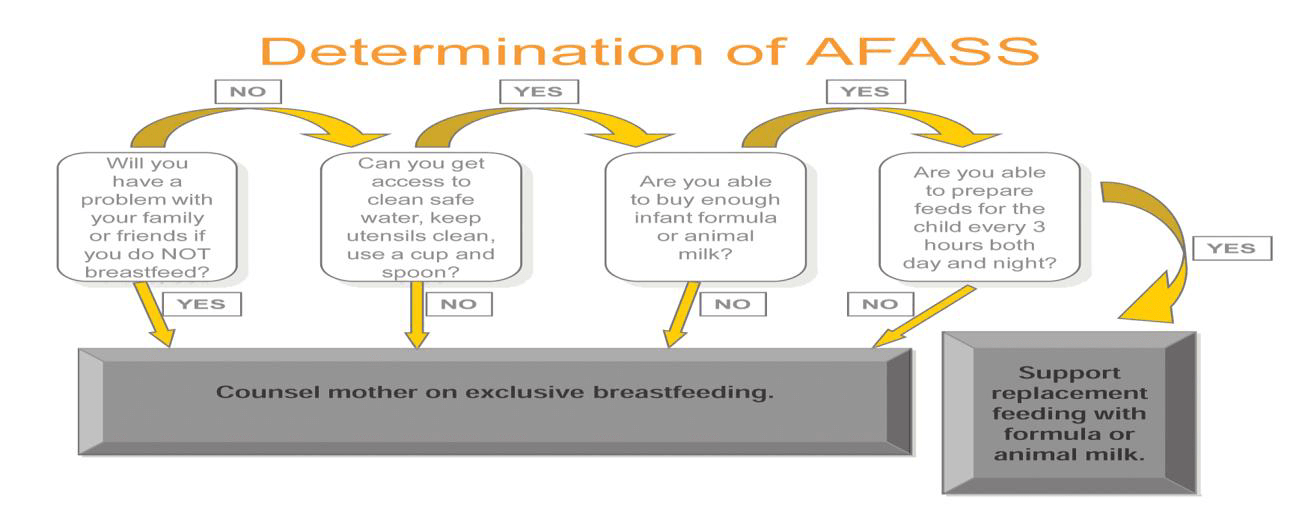
With all these issues in mind the World Health Organization (WHO) has set the following criteria (known as the AFASS criteria), which need to be met before counselling an HIV-positive mother to use formula milk:
If replacement feeding is rejected by the HIV-positive mother, for whatever reasons, there are some things that she can do to reduce the risk of HIV transmission during breastfeeding. Counsel her to:
At six months, if replacement feeding is still not acceptable, feasible, affordable, sustainable and safe, counsel her to continue breastfeeding, but with additional complementary foods. All breastfeeding should stop once a nutritionally adequate and safe diet without breast milk can be provided.